COVID-19 Antibody Testing is Now Available
COVID-19 antibody testing is now available. We are currently use the Catalyst Health Network drive-thru testing sites.
The test is done through a blood sample. You will simply drive up to the testing site at your appointment time and remain in your car. A healthcare team member will be with you to draw your blood. We ask that you remain in your car for 5 minutes before driving off to ensure no lightheadedness. Please come well-hydrated and be sitting on the appropriate side of the car with your preferred arm at the window. You do not need to be fasting for this.
The antibody testing detects the presence of the virus and identifies patients who have been exposed to or recovered from COVID-19. The antibody test is different from the molecular COVID-19 test, which is done with a nasal swab to check for the presence of the COVID-19 virus. After infection with COVID-19, the virus antigen stimulates the immune system to produce antibodies that can be detected in the blood. Antibodies are produced by the immune system after a minimum 10 days of infection and remain positive after the infection. This is why the antibody test can be used to detect a past infection with COVID-19.
Below you will find some answers to some of the frequently asked questions.
How to get tested?
In order to document medical necessity, you will need to undergo a virtual telemedicine visit with one of our providers before the test can be ordered. Once this visit is completed, if you qualify for testing, we will arrange a time and location for you to get your blood drawn and one of our testing sites through Catalyst Health Network.
Who should get tested?
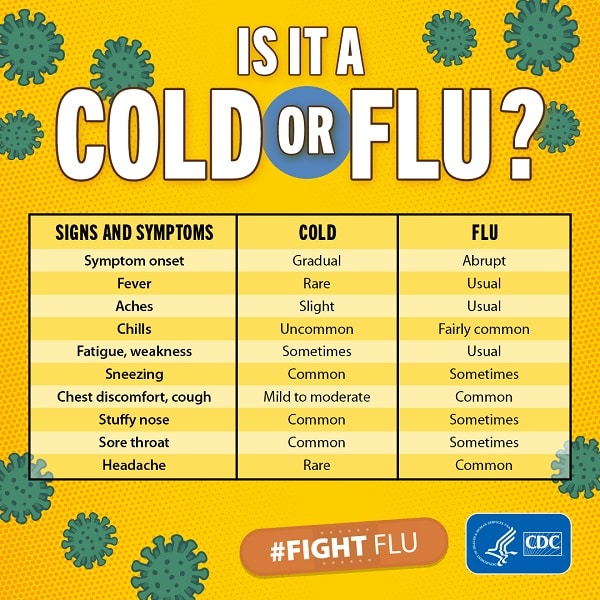
- If you had symptoms (fever, cough, shortness of breath or flu-like symptoms), and want to know whether it was COVID-19 (but should be at least 7 days from onset of symptoms).
- If you are asymptomatic, but may have potentially been exposed (close or proximate contact with a person known to be positive with COVID-19)
- Individuals subject to precautionary or mandatory quarantine
- Individuals employed as a health care worker, first responder, or essential workers who directly interacts with the public
- Individuals present with a case where facts and circumstances warrant testing as determined by clinician or health officials
- If you tested Positive for COVID-19 via Nasal Swab PCR – and want to see if you have produced antibodies that can be detected
Who should not take the test?
Those who are actively having symptoms should not be getting an antibody test done, rather a PCR nasal swab should be done.
If you have had symptoms, please wait at least 7-10 days to take the antibody test, counting from the START of your symptoms. Sensitivity is higher 16-29 days onwards. Antibodies take time to develop – taking the test too early may not give accurate results.
Why should I get tested for COVID-19 antibodies?
Patients who are tested and have the antibodies can use this information in a variety of ways. The risk of getting COVID-19 a second time is suspected to be very low. Individuals who are elderly or have underlying health conditions will benefit from understanding their risk so they can make informed decisions about how much isolation or socialization to resume. The COVID-19 antibody test will also provide important data on the scale of coronavirus infections in our community.
DISCLAIMER: The scientific understanding regarding antibody test interpretation needs further research. Recommendations rely on presumptions made based on experience with similar coronaviruses
What should I do if I have missed or am late for my appointment?
Missed or late arrival will result in forfeiting your appointment. It is important to us that you get the testing that your PCP has recommended! Call the Catalyst Hotline at (214) 964-0319 to let our team know that you have missed or are late to your appointment so we can place you back in queue to be rescheduled according to testing site availability.
What is antibody testing, and how does it differ from diagnostic testing used for COVID-19?
Diagnostic testing for COVID-19 involves looking to see whether an active virus is present. This uses a testing process to detect genetic material from the virus in samples swabbed from the very back of the nasal cavity. This testing is based on a common molecular testing technique: polymerase chain reaction (PCR).
By contrast, antibody testing (also called serology testing) is done with blood samples, because you’re looking for evidence of the body’s immune response to the virus.
After your body is exposed to a foreign pathogen, your white blood cells start to learn about it and make antibodies to neutralize it. So, when an antibody test comes back positive for this coronavirus, it means 1) you were exposed to COVID-19 at some point in the past and 2) your immune system was robust enough to launch an antibody-forming immune response.
What antibodies are tested?
IgM and IgG are tested.
When infected by a virus like COVID-19, the body initially produces antibodies known as IgM (immunoglobulin-M), in an attempt to neutralize the virus. Later, as the body’s adaptive immune system revs up, IgM levels go down, and the body ramps up production of IgG, which more specifically targets the viral invader. IgG ideally is what shows us immunity.
How soon after symptoms can antibodies be detected?
Antibodies can be detected as soon as 7 days after symptom onset. After 7 days, antibodies begin to increase. By day 10-12 after symptom onset, antibodies can be detected in up to 80% of patients and by days 16-29 after symptom onset, antibodies can be detected in all patients.
However, you must note that every person is different. Certain conditions can affect people’s ability to make antibodies, such as: malnourishment, having cancer or another chronic health condition, or taking immune suppressing drugs.
How is the antibody testing done?
The COVID-19 antibody test is a simple blood draw. We then send the sample to our lab and will have results in an average of 1-3 days.
What do Negative antibody test results mean?
A negative antibody test can mean one of these possibilities:
1. You were never exposed
2. Your body has not produced enough antibodies to be detected
3. Your body needs more time to produce antibodies after exposure
4. False negatives – testing limitations.
*Note that some studies show that up to 1/3 of people have low-titers or even absent antibodies after recovering from COVID.
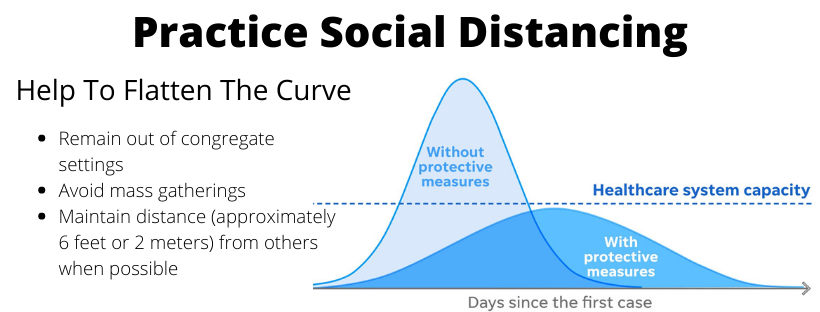
We recommend for you to still wear a mask when in public places, wash your hands on a regular basis and continue to practice social distancing
Please discuss the results with your healthcare provider to discuss your risks and if you are contagious to others.
What do Positive antibody test results mean?
The short answer is we don’t know.
Patients with positive antibody results presumably have been exposed and would be considered low risk for becoming infected.
However, it may mean someone has full immunity or partial immunity or no immunity at all. Some antibodies decrease over time, so you might be immune for six months to a year, and then maybe not at all later on. Or, it might mean where if you get it once, you’re most likely immune the rest of your life. There’s just no way to give definitive answers right now.
A positive antibody test does not mean that you are symptoms free and not able to shed the virus. Please consult your healthcare provider when assessing the results of the antibody test.
We recommend for you to still wear a mask when in public places, wash your hands on a regular basis and continue to practice social distancing
Why is it important for people not to assume they’re immune if they test positive for COVID-19 antibodies?
There’s a big difference between telling someone they have immunity versus that they may have immunity. That’s a really important distinction to make. Because if someone says that they’re definitely going to give me a million dollars, I may go out and buy a new house. But if they tell me they may give me a million dollars, I probably won’t, because it’s not a promise. It’s only potential.
With this virus, we just don’t know the answer yet. We can only advise patients that they may have immunity if the antibody test is positive. So, even if you were to test positive for antibodies to the coronavirus, we recommend for you to still wear a mask when in public places, wash your hands on a regular basis and continue to practice social distancing.
What restrictions/downfall does antibody testing have?
Antibody results:
- are not diagnostic-meaning they cannot be used to diagnose an active infection or tell when a person is no longer contagious.
- do not rule out infection or viral shedding.
- are not a guarantee that you will not get COVID-19.
The antibody testing has not been FDA approved, however the FDA has issued an Emergency Use Authorization (EUA).