Vaccine Safety
Why should I get vaccinated for COVID-19?
COVID-19 can cause serious illness or even death. There’s no way to know how COVID-19 will affect you. And if you get sick, you could spread the disease to friends, family, and others around you, putting their lives at risk. Getting a COVID-19 vaccine greatly reduces the risk that you’ll develop COVID- 19. The vaccines prevent nearly 100% of hospitalizations and deaths due to COVID-19.
Are the COVID-19 vaccines safe?
Yes. The COVID-19 vaccines available in the United States meet the FDA’s rigorous standards for safety and effectiveness. Tens of millions of people in the United States have received COVID-19 vaccines, and all COVID vaccines will continue to be monitored for safety.
Serious health effects from vaccines are very rare. It’s highly unlikely that COVID-19 vaccines will cause long-term health problems. Also, there is no evidence at all that they will cause infertility or cancer.
Your risk for serious health problems is much lower from the vaccine than your risk if you’re unvaccinated and get COVID-19. COVID-19 can leave you with heart and lung damage and other conditions that require long-term treatment. Vaccines are much safer paths to immunity than the disease itself.
How can COVID-19 vaccines be safe since they were developed so fast?
Safe COVID-19 vaccines were developed quickly through the use of a century of vaccine experience; technology that was new to vaccines but had been studied for two decades; a coronavirus vaccine already in development at the National Institutes of Health; and tens of thousands of volunteers for clinical trials that enabled rapid accumulation of data on safety and effectiveness. Simultaneous vaccine production and analysis of testing data also allowed vaccines to be shipped within days of FDA authorization.
Will the shot hurt or make me sick?
No. Some people might get sore muscles, feel tired, or have mild fever after getting the vaccine, but most people report only a sore arm where they got the shot. These reactions mean the vaccine is working to help teach your body how to fight COVID-19 if you are exposed. For most people, these side effects will go away on their own in a few days. If you have any concerns, call your doctor or nurse.
Can the vaccine give me COVID-19?
You can’t get COVID-19 from any of the COVID-19 vaccines in use or being tested in the United States because none of them contains the live virus that causes the disease.
Is it safe for me to get a COVID-19 vaccine if I would like to have a baby one day?
Yes. People who want to get pregnant in the future can receive the COVID-19 vaccine. Experts believe that COVID-19 vaccines are unlikely to pose a risk to a person trying to become pregnant in the short or long term.
Are the COVID-19 vaccines safe for people who are pregnant?
Yes. If you’re pregnant, you may choose to be vaccinated when it’s available to you. There’s currently no evidence that antibodies formed from COVID-19 vaccination cause any problem with pregnancy, including the development of the placenta.
People who are trying to become pregnant now or who plan to try in the future may receive the COVID-19 vaccine when it becomes available to them. There’s no evidence that fertility problems are a side effect of any vaccine, including COVID-19 vaccines. There’s no routine recommendation for taking a pregnancy test before you get a COVID-19 vaccine.
If you have questions about getting vaccinated, talk with your health care provider.
Why are people having allergic reactions to the COVID-19 vaccines?
A few people have had allergic reactions called anaphylaxis after getting a COVID-19 vaccine but were treated and have recovered. Your doctor can help you decide if it’s safe for you to be vaccinated
Are the COVID-19 vaccines safe for people with certain underlying medical conditions?
COVID-19 vaccines may be administered to most people with underlying medical conditions. If you have questions about getting a COVID-19 vaccine, talk with your health care provider. Inform your vaccination provider about all your allergies and health conditions.
Vaccine Effectiveness
How do COVID-19 vaccines work?
Vaccines train your immune system to recognize and fight the virus that causes COVID-19. With vaccines, you can build immunity to a disease without getting the disease.
How effective are the COVID-19 vaccines?
All FDA-authorized COVID-19 vaccines are highly effective at preventing severe illness, hospitalization, and death due to COVID-19, including from the Delta variant.
Remember: You’re not fully protected from COVID-19 unless you’re fully vaccinated.
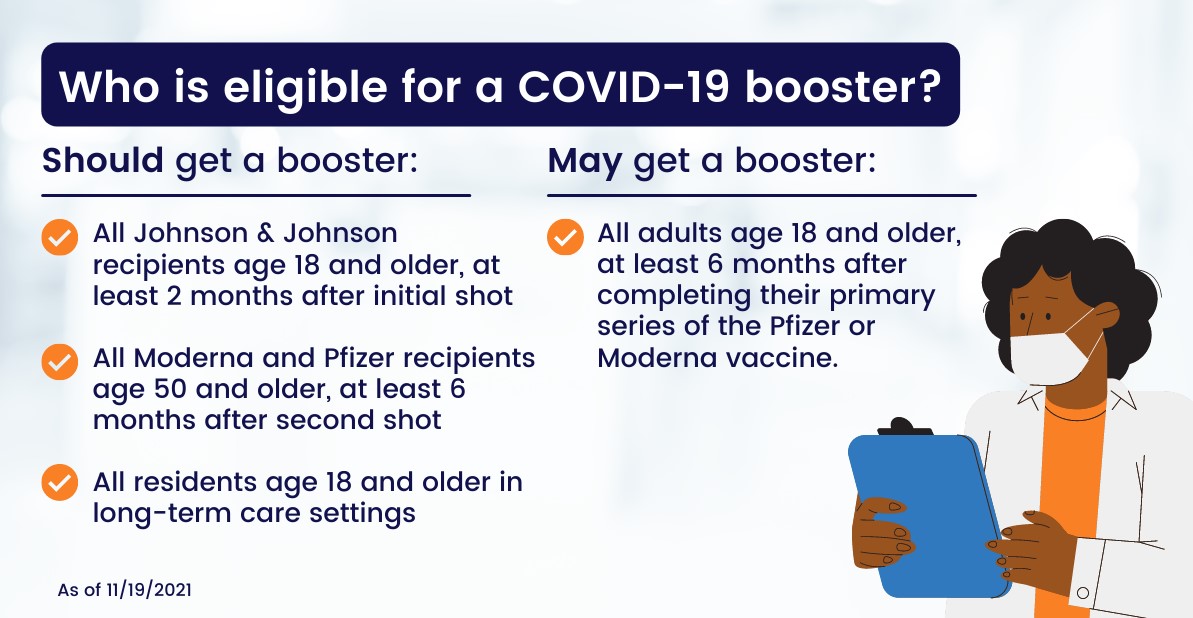
Johnson & Johnson’s Janssen vaccine requires one dose.
The Pfizer-BioNTech and Moderna vaccines require two doses.
Why should I get vaccinated if I can still get infected with COVID-19?
It’s important to understand that infection doesn’t necessarily lead to illness. If you’re fully vaccinated against COVID-19 and the virus manages to enter your body and begins to multiply— that is, infect you—your immune system will be prepared to quickly recognize the virus and keep it from doing real damage. That’s why most people who get infected with COVID-19 despite being vaccinated—so-called breakthrough cases—have no symptoms (asymptomatic) or only mild-to-moderate illness.
Nearly everyone in the United States who is getting severely ill, needing hospitalization, and dying from COVID-19 is unvaccinated.
CDC recommends you get vaccinated as soon as you can.
How long do COVID-19 vaccines last?
Scientists don’t know right now how long COVID-19 vaccines protect people, but they are investigating this in medical studies.
Do I need to get a COVID-19 vaccine if I’ve already had COVID-19?
Yes. Scientists don’t yet know how long natural antibodies in people who have had COVID- 19 will be protect them from being reinfected.
Will the COVID-19 vaccines prevent me from infecting others?
COVID-19 vaccines reduce the likelihood that you’ll develop and be able to spread COVID-19. In rare occasions, some vaccinated people can get COVID-19 from the highly contagious Delta variant and spread it to others. Importantly, only a very small amount of spread happening around the country comes from vaccinated individuals.
Do the vaccines work on the new COVID variants?
Scientists continue to study different forms, or variants, of the virus that causes COVID-19 to see if the vaccines will work against them. Current data suggest that COVID-19 vaccines authorized and recommended for use in the United States offer protection against most variants, including the highly contagious Delta variant. For this reason, COVID-19 vaccines are an essential tool to protect people against COVID-19, including illness caused by the new variants. CDC will continue to monitor the impact these new variants may have on how well the vaccines work.
Do I need to wear a mask after getting vaccinated?
If you’re fully vaccinated, you can participate in many of the activities that you did before the pandemic. To maximize protection from the highly contagious Delta variant and prevent possibly spreading it to others, wear a mask inside public places if you’re in an area of substantial or high spread of COVID-19.
If you’re not yet vaccinated, you should continue to:
- Wear a mask when inside public places.
- Keep at least 6 feet part from people who don’t live with you and who may not be vaccinated.
- Avoid crowds.
- Avoid poorly ventilated spaces.
- Wash your hands with soap and water for at least 20 seconds or use alcohol-based hand sanitizer when soap and water are not available.
Vaccinated and unvaccinated people must still follow federal, state, local, tribal, and territorial laws, rules, and regulations. That includes public transportation, airport/airplane, local business, and workplace guidance.
Also, if you have a medical condition or you take medicines that weaken your immune system, you may not be fully protected from COVID-19 even if you’re fully vaccinated. Talk to your health care provider. Even after vaccination, you may need to continue taking precautions.